Conventional IVF
Procedure of conventional IVF (In Vitro Fertilization / Test Tube Fertilization)
1. Pretreatment with medication
In conventional IVF, drug pretreatment is used to ensure that a relatively high number of eggs are produced. For this purpose, usually 150 – 225 I.U. FSH (Gonal-F or Puregon) or a FSH/LH mixture (Menogon) is injected subcutaneously (under the skin) every day. Depending on the stimulation protocol, various drugs are also needed to prevent premature ovulation (Synarela spray, Zoladex, Enantone, Dekapeptyl).

When enough follicles (egg sacs) have grown, the so-called “ovulation injection” (Brevactid, Pregnesin, Ovitrelle) is administered to complete the egg maturation phase. Now the eggs have to be retrieved.
2. Egg collection
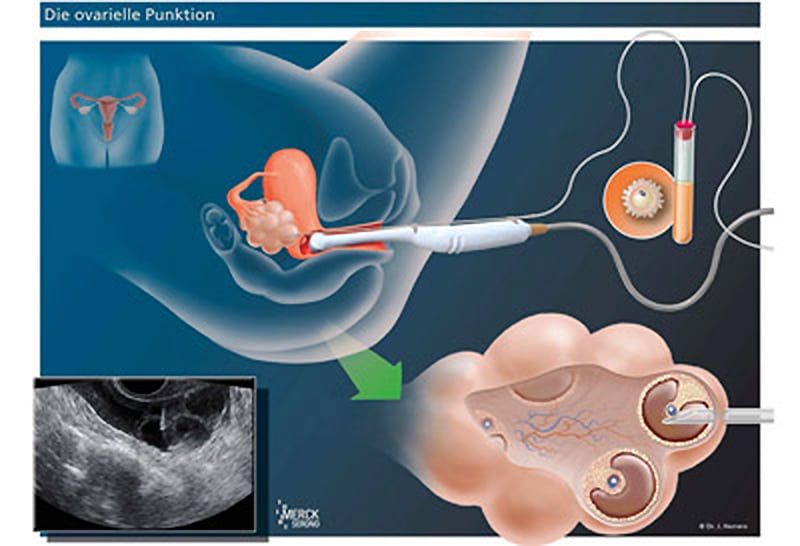
Vaginal follicular puncture under ultrasound guidance is usually done under a short anesthesia 32 to 36 hours after HCG injection.
During this procedure, a puncture needle is inserted into the vagina in a guide sleeve on the ultrasound probe. The ovary is only a few millimeters away. The needle is now inserted through the vaginal wall directly into the individual follicles. The fluid is aspirated and passed directly to the biologist so that it can be determined immediately whether there is an egg in it.
3. Fertilisation
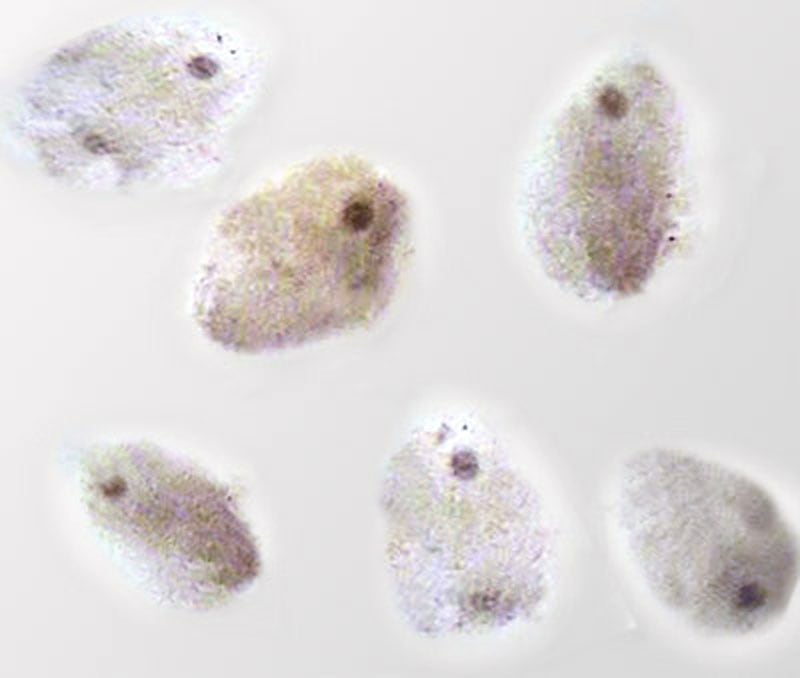
The oocytes are placed in nutrient solution in the laboratory and overlaid with approximately 50 000 – 100 000 well-motile sperm. The dishes are then “incubated” ( cultured) overnight in the incubator.
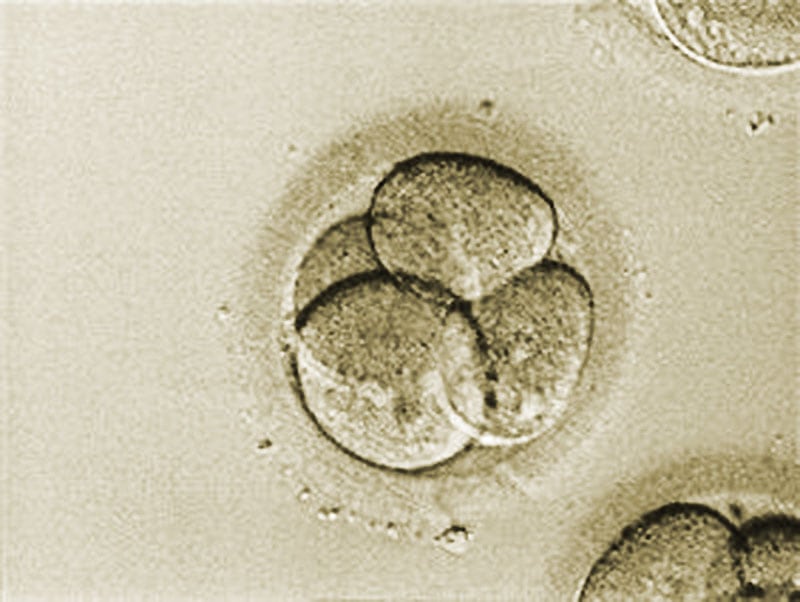
After 19-21 hours later it is determined how many eggs have reached the so-called pronucleus stage (PN stage-Pro Nucleus), it must be selected (at least in Germany) which PN stage cells (max. 3) should complete the fertilization process. The pronuclei each contain the chromosomes of the egg cell and the sperm cell.

A so-called 2PN cell (pronuclear cell nucleus)On the 2nd or 3rd day after sperm addition, when one or more embryos have developed, the embryo(s) are transferred to the uterine cavity. Transfer on the 5th day is also possible and useful if one or more blastocysts have developed.


More information about blastocyst transfer.
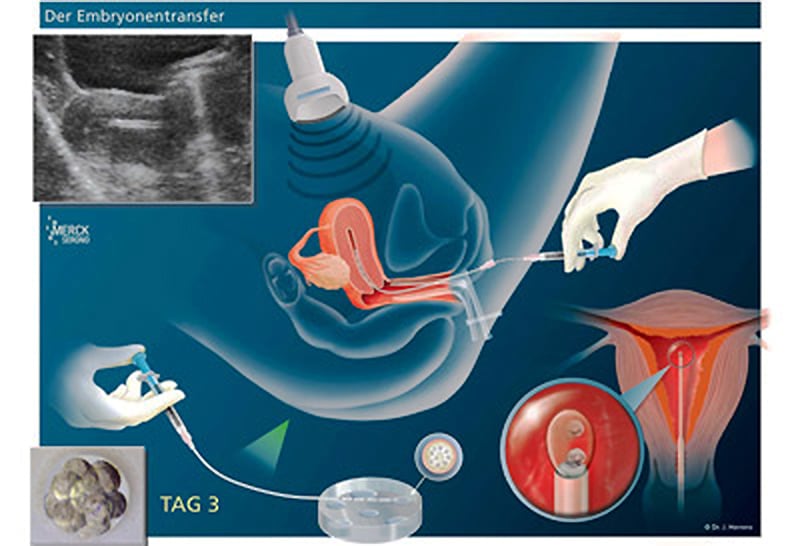
4. Embryo transfer
On the 2nd, 3rd or 5th day after sperm addition, embryo transfer is performed. In this procedure, a catheter is inserted into the uterine cavity completely painlessly, if necessary under ultrasound control. The embryo(s) is/are carefully deposited there.
In preparation for this transfer, the woman may take medication that calms the uterine muscles. Over the following 14 days, by adding progesterone (luteal hormone: Crinone gel, Utrogest) , optimal mucosal conditions for implantation (implantation) of the embryo should be achieved.

In the period after embryo transfer, excitement and too much activity should be avoided, as well as circulatory stress, e.g. through sports and strong temperature increases, e.g. sauna visits, hot tub baths. Otherwise, there are no special recommendations to be made. Sex also tends to have a positiv effect.
12 to 14 days after fertilization, a urine pregnancy test or blood test can determine whether the woman is pregnant.
One advantage of this method is that there are usually “enough” (partially) fertilized eggs “left over”, which can then be used in later “cryo cycles“.
However, recent studies indicate that the percentage of “good” oocytes seems to be higher when fewer oocytes are grown. This would mean that there are fewer viable cells among the frozen cells (obtained in conventional IVF) than expected and hoped for.
Risks of IVF
- OHSS
- Organ injury
- Multiple pregnancy
- Ectopic pregnancy
OHSS does not occur with NC-IVF and Mini-IVF.
OHSS (Ovarian Hyper Stimulation Syndrome)
With any hormonal stimulation of the ovaries, as undertaken during pre-treatment in the course of in vitro fertilization and intracytoplasmic sperm injection, there is a risk of ovarian hyperstimulation. The higher the stimulation dose chosen, the higher the risk of overstimulation. The risk is particularly high for stimulation of women with PCO syndrome.
The aim of ovarian stimulation for IVF is to achieve maturation of several oocytes in order to obtain sufficient embryos for embryo transfer with sufficient probability. At the standard dose of 150-225 I.U. FSH per day usually chosen, the targeted 10-15 follicles grow. However, especially during the first stimulation cycle, it is not yet known how exactly the woman will react to the hormone administration. If the reaction is too strong, OHSS can be the result. In OHSS, often 20-50 follicles grow, which by their size alone cause corresponding pressure discomfort. Just imagine that a mature follicle has a diameter of 2 cm. An additional problem arises from the estrogen production of the follicles. The higher the blood level, the more the vessel walls change and sometimes extreme fluid shifts (from the blood to the abdominal cavity), further increasing the pressure complaints. This fluid accumulation (ascites) can become so severe that a pronounced feeling of illness and, due to the relative lack of water in the blood, a risk of thrombosis develops. The accumulation of water can be suctioned transvaginally (through the vagina as in follicular puncture) or percutaneously (through the skin) in order to achieve a rapid improvement of the symptoms. Unfortunately, this usually has to be performed several times, over several days, as the permeability of the vascular walls persists.
In extreme cases, intensive medical care may be required.
Follicular punture – egg collection
Follicular puncture is performed under vaginal sonographic view without – or with – anesthesia. The use of local anesthesia is also possible, but not without effort.
During the puncture, a long needle is passed through a guide rail attached to the ultrasound probe. Under visual control, the needle is then inserted through the vaginal wall (2-3mm) directly into the follicle, in whose fluid the egg cell is located. If the ovary is in an unfavorable position or there are other technical problems, injury to the intestine, blood vessels and bladder is possible.
Since the procedure is performed through the vagina, there is a general risk of infection, even if local disinfection is performed.
Multiple pregnancy
In order to achieve pregnancy rates of 30-35% in Germany, on average at least 2 embryos must be transferred. The multiple pregnancy rate in Germany is about 20-25%, that of a triplet pregnancy up to 4%. The problem is the increase of pregnancy complications, -early birth and the resulting problems.
For years, the – unintended – multiple pregnancy has been considered a failure of reproductive medicine. There are several ways to reduce this risk, but many of them are prohibited in Germany. In countries with much more liberal legislation, comparable pregnancy rates are already achieved after transfer of only one “top quality” embryo.
A SET (Single Embryo Transfer) is an optimal prevention strategy for multiple pregnancies under liberal legislation and with the appropriate expertise of the IVF laboratory.
EU (extrauterine pregnancy)
Even with IVF, ectopic pregnancy can occur because the embryos move back and forth in the uterine cavity (due to muscle contractions) for several days. Thus, it can happen in up to 4% that they move up to the fallopian tube and lead to the complication-laden EU. Depending on the time of diagnosis, this is treated either with medication or surgery. Only early diagnosis can protect against life-threatening complications.
— Diagrams: © Professor Herrero, Barcelona
