IUI
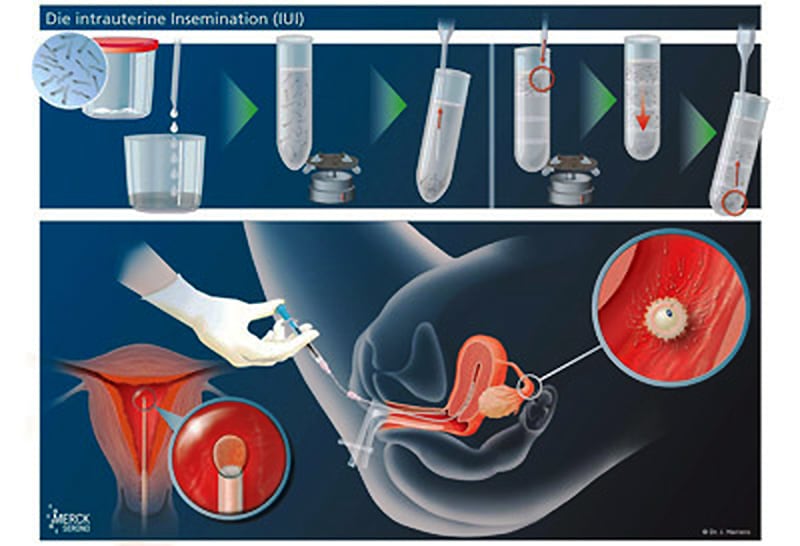
Insemination is one of the comparatively simple procedures and is performed in cases of rather mild limitations of male fertility or disorders in the cervical canal, e.g. disorders of mucus formation or condition after conization (conical section of the external cervix). The treatment can be carried out with or without hormone treatment, depending on the possible presence of oocyte maturation disorders. The purpose of this treatment is to bring a high concentration of prepared sperm close to the egg in order to promote fertilization.
Therapy in the natural cycle
If a woman’s cycle is regular, it can be assumed that a follicle (egg sac) is growing in which the egg cell is maturing. Typical changes in the endometrium and hormone levels provide information about the status of this development. With one or two ultrasound examinations and close hormone monitoring, the time/day of ovulation can usually be accurately predicted. Insemination (sperm transfer) can then be carried out on the determined day. However, this requires a high degree of flexibility on both sides, since the body’s own rhythm dictates the schedule. It is better to “schedule” ovulation. This also results in an automatic improvement of the corpus luteum phase.
After reaching a follicle size of about 18 – 20 mm, ovulation can be specifically induced with the “ovulation syringe”. Approximately 32 – 36 hours later, the sperm can be transferred into the uterine cavity after appropriate preparation (Intra uterine Insemination – IUI). Pregnancy rates can be reported as a maximum of 10 – 15% (20?) per treatment cycle. Intravaginal insemination has no advantages over natural sexual intercourse and therefore has no therapeutic significance. Since cysts are rarely expected after such a cycle, every cycle can be used.

IUI in a stimulated cycle
As explained in the section on Hormone treatment, drugs are used to correct a wide range of hormonal imbalances.
Hormonal stimulation for IUI (intra-uterine insemination / sperm transfer) is used when there is no independent follicle development (follicle maturation) leading to a “jumping follicle” (mature follicle).
Clomifene stimulation
The simplest stimulation is done with the active ingredient clomifene citrate, often abbreviated CC. These tablets are usually taken over a period of 5 days from the 5th – 9th day of the cycle and result in an increase in FSH production (follicle stimulating hormone). Follicle growth (follicles) is monitored by ultrasound and, if necessary, by hormone tests in the blood.
After reaching a follicle size of about 18 – 20 mm, ovulation can be specifically induced with the “ovulation syringe”. About 32 – 36 hours later, the sperm can be transferred into the uterine cavity after appropriate preparation (Intra uterine Insemination – IUI). Pregnancy rates can be reported as a maximum of 10 – 15% (20?) per treatment cycle. Intravaginal insemination has no advantages over natural sexual intercourse and therefore has no therapeutic significance.
NOTE: The public health insurance companies subsume insemination under clomiphene stimulation under UNSTIMULATED cycles. This must be taken into account when applying for cost coverage (partial coverage).
FSH stimulation
If clomiphene stimulation has been unsuccessful (no follicle growth or merely no pregnancy success), FSH (follicle stimulating hormone) can be injected daily under the skin. This is usually done from the 3rd – 11th/12th day of the cycle. The direct supply of FSH usually has a good effect, but more often than with clomiphene stimulation, more than one follicle matures. Therefore, at least FSH stimulation therapy belongs in the hands of a specialist.
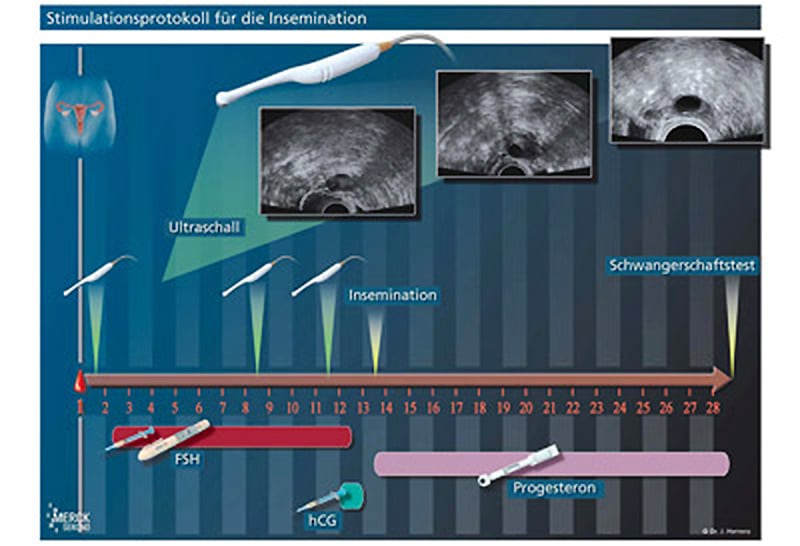
After reaching a follicle size of about 18 – 20 mm, ovulation can be specifically induced with the “ovulation syringe”. Approximately 32 – 36 hours later, the sperm can be transferred into the uterine cavity after appropriate preparation (intra uterine insemination – IUI). Pregnancy rates can be reported as a maximum of 10 – 15% (20?) per treatment cycle. Intravaginal insemination has no advantages over natural sexual intercourse and therefore has no therapeutic significance.
— Diagrams: © Prof. Herrero, Barcelona








