IUI
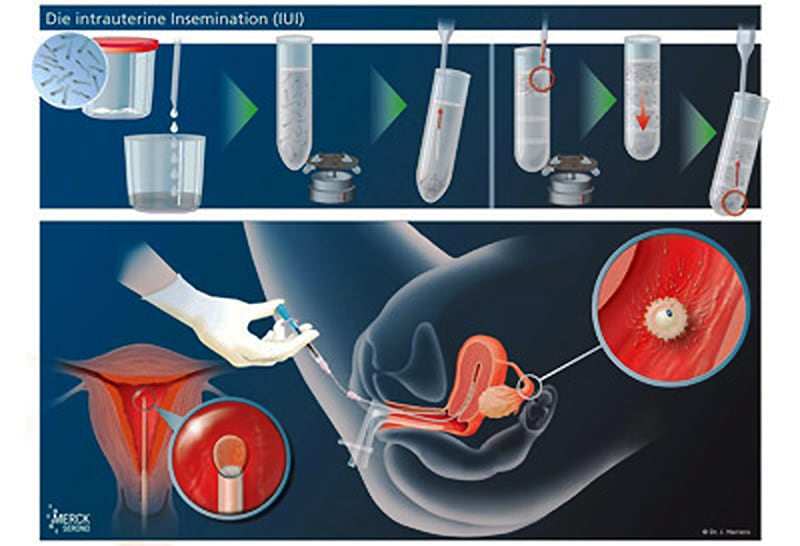
Die Insemination gehört zu den vergleichsweise einfachen Verfahren und wird bei eher leichteren Einschränkungen der männlichen Fertilität oder bei Störungen im Gebärmutterhalskanal, z. B. Störungen der Schleimbildung oder bei Zustand nach Konisation (Kegelschnitt des äußeren Muttermundes), durchgeführt. Die Behandlung kann je nach eventuell vorliegender Eizellreifungsstörung mit-, aber auch ohne Hormonbehandlung erfolgen. Sinn dieser Behandlung ist es, die aufbereiteten Spermien in hoher Konzentration in die Nähe der Eizelle zu bringen, um das Eintreten einer Befruchtung zu fördern.
Therapie im natürlichen Zyklus
Bei einem regelmäßigen Zyklus der Frau ist davon auszugehen, dass es zum Heranwachsen eines Follikels (Eibläschens) kommt, in dem die Eizelle heranreift. Typische Veränderungen der Gebärmutterschleimhaut und der Hormonwerte geben Aufschluß über den Stand dieser Entwicklung. Durch ein bis zwei Ultraschalluntersuchungen und eine engmaschige Hormonkontrolle lässt sich der Zeitpunkt/Tag des Eisprungs meist genau vorhersagen. Dann kann am entsprechend ermittelten Tag die Insemination (Samenübertragung) durchgeführt werden. Dies setzt jedoch ein Höchstmaß an Flexibilität von beiden Seiten voraus, da ja der körpereigene Rhythmus den Zeitplan vorgibt. Besser ist es, den Eisprung zu „terminieren“. Dies hat auch eine automatische Verbesserung der Corpus luteum- (Gelbkörper-) phase zur Folge.
Nach Erreichen einer Follikelgröße von etwa 18 – 20 mm kann mit der „Eisprungspritze“ der Eisprung gezielt ausgelöst werden. Etwa 32 – 36 Stunden später können die Spermien nach einer entsprechenden Präparation in die Gebärmutterhöhle übertragen werden (Intra uterine Insemination – IUI). Die Schwangerschaftsraten können mit maximal 10 – 15 % (20?) pro Behandlungszyklus angegeben werden. Die intravaginale Insemination hat keine Vorteile gegenüber dem natürlichen Geschlechtsverkehr und hat daher keine therapeuthische Bedeutung.
Da nach einem solchen Zyklus Zysten nur selten zu erwarten sind, kann jeder Zyklus genutzt werden.

IUI im stimulierten Zyklus
Wie unter Hormonbehandlung erläutert, kommen bei verschiedensten hormonellen Ungleichgewichten Medikamente zur Anwendung, welche die Störungen beheben sollen.
Die hormonelle Stimulation zur IUI (Intra-uterine-Insemination / Samenübertragung) kommt zum Einsatz, wenn es keine selbstständige Follikelentwicklung (Eibläschenreifung) gibt, die zu einem „sprungreifen Follikel“ (reifes Eibläschen) führt.
Clomifenstimulation
Die einfachste Stimulation erfolgt mit dem Wirkstoff Clomifencitrat, oft CC abgekürzt. Die Einnahme dieser Tabletten erfolgt meist über 5 Tage vom 5. – 9. Zyklustag und hat eine Erhöhung der FSH Produktion (Follikel stimulierendes Hormon) zur Folge. Das Follikelwachstum (Eibläschen) wird per Ultraschall, gegebenenfalls auch durch Hormonuntersuchungen im Blut, kontrolliert.
Nach Erreichen einer Follikelgröße von etwa 18 – 20 mm kann mit der „Eisprungspritze“ der Eisprung gezielt ausgelöst werden. Etwa 32 – 36 Stunden später können die Spermien nach einer entsprechenden Präparation in die Gebärmutterhöhle übertragen werden (Intra uterine Insemination – IUI). Die Schwangerschaftsraten können mit maximal 10 – 15 % (20?) pro Behandlungszyklus angegeben werden. Die intravaginale Insemination hat keine Vorteile gegenüber dem natürlichen Geschlechtsverkehr und hat daher keine therapeuthische Bedeutung.
ANMERKUNG: Die gesetzlichen Krankenkassen subsummieren die Insemination unter Clomifenstimulation unter UNSTIMULIERTE Zyklen. Dies ist zu beachten bei der Beantragung der Kostenübernahme (Teilübernahme).
FSH Stimulation
Ist die Clomifenstimulation bisher erfolglos geblieben (kein Follikelwachstum oder lediglich kein Schwangerschaftserfolg), kann täglich FSH (Follikel stimulierendes Hormon) unter die Haut gespritzt werden. Dieses erfolgt meist vom 3. – 11./12. Zyklustag. Die direkte Zufuhr von FSH hat meist eine gute Wirkung, jedoch kommt es hierbei häufiger als bei der Clomifenstimulation zum Heranreifen von mehr als einem Follikel (Eibläschen). Daher gehört zumindest die FSH Stimulationstherapie in die Hand des Spezialisten.
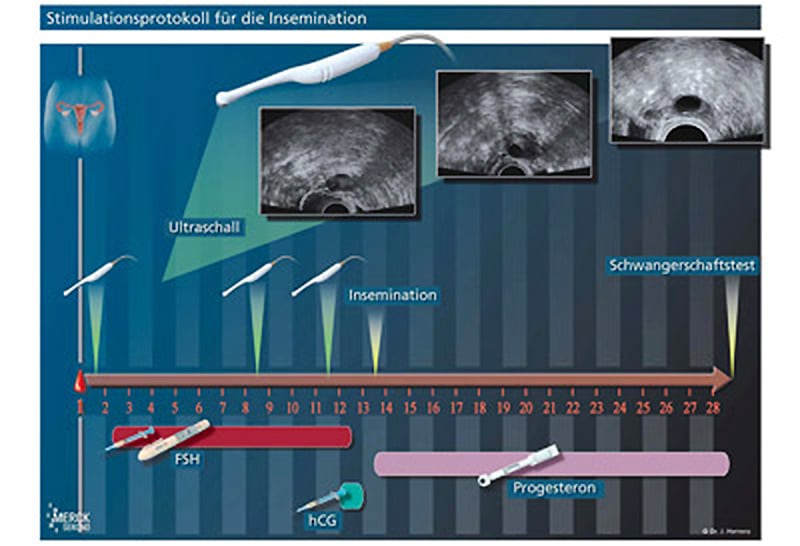
Nach Erreichen einer Follikelgröße von etwa 18 – 20 mm kann mit der „Eisprungspritze“ der Eisprung gezielt ausgelöst werden. Etwa 32 – 36 Stunden später können die Spermien nach einer entsprechenden Präparation in die Gebärmutterhöhle übertragen werden (Intra uterine Insemination – IUI). Die Schwangerschaftsraten können mit maximal 10 – 15 % (20?) pro Behandlungszyklus angegeben werden. Die intravaginale Insemination hat keine Vorteile gegenüber dem natürlichen Geschlechtsverkehr und hat daher keine therapeuthische Bedeutung.
—
Schematische Darstellungen: © Prof. Herrero, Barcelona









